
Practice Perfect 864
Recognizing Opioid Abuse
Recognizing Opioid Abuse

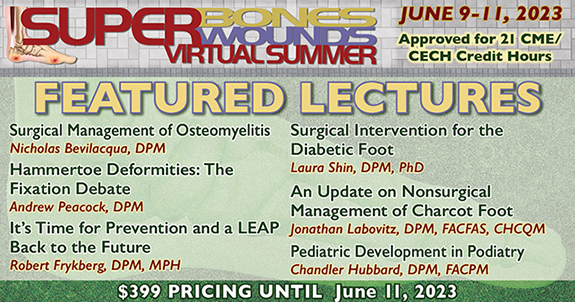
As many of you may have seen, the DEA is requiring training in opioid prescribing, and PRESENT e-Learning has responded to this need with the DEA Required Substance Use Disorder Training Course, a new virtual series and upcoming on-demand course to educate providers and keep us compliant with the law. I’m especially happy for the additional June 25th session to help those of us on the West coast. In honor of this new virtual course, the Practice Perfect editorial is re-releasing a past issue about recognizing opioid abuse in our patients. I hope you find this evidence-based issue to serve as a good companion to the virtual conferences.
In my practice, there’s a tight race between opioids and antibiotics as my most common prescriptions. Obviously, each one has its own issues, but pound for pound, I spend more of my time worrying about opioid complications than antibiotics. If we get past the allergic response, diarrhea, and pseudomembranous colitis, antibiotics aren’t that big a deal. But opioids are.
I know, I’m being a little facetious here. Clearly we have to be worried about the potential complications associated with antibiotics. However, prescribing opioids presents its own difficulties. For those of us prescribing these medications, the real problem comes in balancing between prescribing for legitimate patients versus those seeking pain medications due to addiction.
If physicians had a reliable way to “read” our patients for the presence of opioid addiction, it would give us the ability to make decisions, which we currently lack today. For example, if I prescribe hydrocodone for a patient who underwent surgery, and he becomes addicted to this medication, then I might have repaired the acute issue that required the surgery but would have created a new long-term medical problem. Although unintentional, this result is clearly not following the dictum of primum non nocere, first, do no harm. On the other hand, denying a patient in legitimate pain needlessly prolongs suffering.
If we somehow had a test – say a blood test that determined a patient’s opioid addiction level – we would have the ability to do a number of things: decline a prescription, alert pharmacies, speak with the primary care physician, begin a referral for addiction treatment, or work to prevent overdose and potentially death. A physician could choose to do all or some of these things. Of course, we don’t have the luxury of such a test. We are then left with the highly subjective task of figuring out if our patients are addicted to their pain medications or are truly in pain.
The Centers for Disease Control and Prevention recently published a study looking at the risk factors for patients on acute opioids to convert to chronic use1. Researchers took a random sample of patient records from 2006 – 2015 from the IMS Lifelink+ database, which aggregated insurance information. They looked at data from patients 18 years or older who had been prescribed at least one opioid during the study period. Using Kaplan-Meier survivor statistics they found almost 1.3 million people who met their inclusion criteria and determined the following results of people who continued opioid therapy for greater than one year:
- More likely to be a female, older, and have a pain diagnosis before opioid initiation.
- Of those prescribed at least one day of opioids the probability of continued use at one year was 6.0% and at three years was 2.9%.
- Median time to discontinuation was seven days.
- The largest increases in probability of continued use was noted when: the first prescription exceeded 10 or 30 days, the patient received a third prescription, or when the cumulative dose exceeded 700 mg morphine equivalents.
- Prescribing long-acting opioids and tramadol at initial treatment also lead to significantly higher continued use at one and three years.
The authors concluded that one day of opioid did not increase the risk of long term use, but the greatest risk of continued opioid use was noted if the initial prescription was greater than eight days (13.5%) and greater than one month (29.9%). They also found that one in seven patients who received a refill or had a second opioid prescription were on this medication one year later.
One day of opioid did not increase the risk of long term use, but the greatest risk of continued opioid use was noted if the initial prescription was greater than eight days (13.5%) and greater than one month (29.9%). One in seven (14%) patients who received an opioid refill or had a second opioid prescription were on this medication one year later. Prescribing greater than one week’s worth of opioids doubles the chances of continued use at one year.
They recommended prescribing opioids for acute pain for periods less than seven days (ideally less than three days) and to be highly cautious when prescribing for greater than this period as prescribing less than one week’s worth of opioids doubles the chances of continued use at one year.
Although I understand the significance of these findings and the recommendations to minimize the dose and time-frame of opioids, I find myself in the bind of having to prescribe pain medications for longer time-frames than recommended here. Foot and ankle surgery may be painful for some patients, often requiring more than a week’s worth of opioids. Preemptive analgesia with preoperative regional blockade is helpful but does not eliminate the issue. National guidelines such as those established by pain physicians2 are often helpful. However, they don’t help us identify which of those patients are malingering and which are legitimate. Unfortunately there’s no final answer on this.
Here are a few hints from the literature to help determine and/or recognize a patient’s opioid abuse:
Risk Factors for Opioid Abuse:
- History of psychiatric disease such as mood disorder, depression, psychosocial problems3 increases the risk of dependence.
- History of prior substance use disorder3 also increases the risk of dependence.
- Concurrent use of other recreational drugs (ex, Cocaine) is associated with opioid dependence4. Check urine drug tests (UDT) for this phenomenon.
- Notice the 3 Cs of addiction5:
• Loss of Control – Reports lost or stolen Rx, calls for early refills, seeking opioids from other sources, physical signs of withdrawal at appointments.
• Craving – Repeated requests for increased doses, increased pain despite non-progression of disease, dismissive of non-opioid treatments.
• Consequences (patient suffers negative effects but continues to use) – Somnolence, decreased activity or function.
Striking the balance between under-prescribing (and leaving our patients in pain) and over-prescribing (contributing to addiction) is one of the most difficult parts of medical care. Hopefully, future research will improve our predictive ability, but until then I hope these suggestions help out, if only a little.
Best wishes.

Jarrod Shapiro, DPM
PRESENT Practice Perfect Editor
[email protected]

-
Shah A, Hayes CJ, Martin BC. Characteristics of Initial Prescription Episodes and Likelihood of Long-Term Opioid Use - United States, 2006-2015. Morb Mortal Wkly Rep. 2017;66:265-269.
Follow this link -
Manchikanti L, Kaye, AM, Knezervic NN, et al. Responsible, Safe, and Effective Prescription of Opioids for Chronic Non-Cancer Pain: American Society of Interventional Pain Physicians (ASIPP) Guidelines. Pain Physician. 2017;20: S53-92.
Follow this link -
Kaye AD, Jones MR, Kaye AM. Prescription Opioid Abuse in Chronic Pain: An Updated Review of Opioid Abuse Predictors and Strategies to Curb Opioid Abuse: Part 1. Pain Physician. 2017 Feb;20(2S):S93-S109.
Follow this link -
Kaye AD, Jones MR, Kaye AM. Prescription Opioid Abuse in Chronic Pain: An Updated Review of Opioid Abuse Predictors and Strategies to Curb Opioid Abuse: Part 2. Pain Physician. 2017 Feb;20(2S):S111-S133.
Follow this link -
Manchikanti L, Atluri S, Trescot AM, Giordano J. Pain Physician 2008; Opioids Special Issue. Pain Physician. 2008;SI55-SI80.
Follow this link


























Comments
There are 0 comments for this article